Glaucoma Center



Glaucoma
Glaucoma is one of the leading causes of vision loss and blindness in the U.S. It is a condition which causes ongoing damage to the optic nerve, which sends signals from the eye to the brain. This damage results in blind spots in the peripheral vision which expand over time and lead to blindness if not treated. There are many effective treatments which will prevent blindness in most people, especially if the condition is detected early.
What causes glaucoma?
We do not know the exact reasons people get glaucoma, but high eye pressure appears to be the main cause for damage to the optic nerve. Glaucoma tends to run in families and is more common in certain ethnic groups. Older age is another important risk factor.
How can I get tested for glaucoma?
A regular eye exam at your doctor’s office will help determine if you are at risk for glaucoma. Your doctor will examine your optic nerves, measure your eye pressures, and ask if glaucoma runs in your family. If you are found to be at risk for glaucoma, your doctor may get additional tests. One is called an “OCT,” which takes a high definition scan of your optic nerves to find areas of glaucoma damage. Another is a “visual field test,” which checks your peripheral vision for any blind spots. You may also have a photograph taken of your optic nerves, which can be used to check for any changes in appearance in the future. If you are found to have glaucoma and started on treatment, these tests will be repeated over time to make sure your glaucoma is not getting worse.
What are the symptoms of glaucoma?
Typically glaucoma progresses slowly and without any symptoms, which makes regular eye exams and screening tests important to detect it. Patients usually do not notice any blind spots until they have had a lot of damage to their optic nerves. A rare type of glaucoma, called “acute angle closure,” can suddenly cause very high eye pressures which lead to pain, headache, nausea, vomiting, haloes, and vision loss.
How is glaucoma treated?
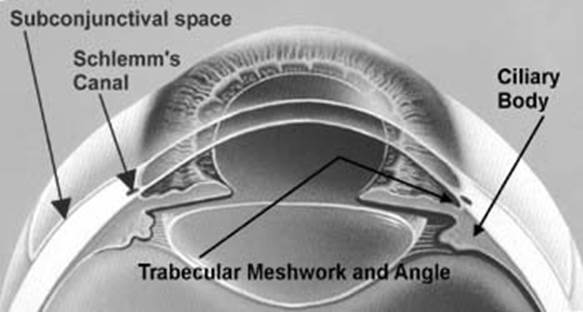
Glaucoma is treated by lowering eye pressure with eye drops, lasers, or surgery. Your doctor will determine how low your eye pressure needs to be to protect your optic nerve. Most patients will be started on an eye drop that is taken once or twice every day. Sometimes several different eye drops are needed. For most people, the eye drops are very effective. If eye drops don’t lower the eye pressure enough, laser trabeculoplasty may be performed. The laser, which is administered in a few minutes as an outpatient, allows the fluid in the eye to drain more easily, which lowers pressure. If the drainage angles are narrow or closed, laser peripheral iridotomy (LPI) will be performed to create a new opening for fluid to get to the eye’s natural drain.
Finally, surgery can lower eye pressure if eye drops and laser do not. Certain “Minimally Invasive Glaucoma Surgeries (MIGS)” may lower your pressure with less risk than conventional surgeries. Your doctor will determine if you are a good candidate for these. The most effective surgery to lower eye pressure is called a trabeculectomy. Trabeculectomy involves creating an alternate pathway for fluid to drain out of the eye, usually under the upper eyelid. Most patients have a good result with a lower pressure from this surgery. Risks of the surgery include having too low of a pressure and getting an eye infection, both of which can cause vision loss. A similar surgery, called a tube shunt, involves inserting a small tube inside the eye which allows fluid to drain under the upper eyelid.
